What Is Provider Credentialing in Healthcare?
Provider credentialing in healthcare is the process by which medical organizations verify the credentials of healthcare providers to ensure they have the required licenses, certifications, and skills to properly care for patients.
The process is also called physician credentialing, medical credentialing, or doctor credentialing. Healthcare credentialing is most often associated with the process of authorizing physicians, but similar — although sometimes less extensive — systems are in place for nurses and other healthcare providers.
Credentialing by Other Names
Credentialing in the healthcare industry sometimes goes by other terms, including the following:
- Insurance Credentialing: Also known informally as “getting on insurance panels,” this term refers to a health insurance company verifying a physician’s credentials. Every health insurance company checks the credentials of a physician before it includes the doctor as an in-network provider.
- Paperless Credentialing: This term refers to software that expedites the credentialing process, decreasing or eliminating the need for paper forms.
- Medical sales rep credentialing: Also known as vendor credentialing, this refers to healthcare organizations checking on and monitoring the background and training of sales reps and other vendors who may want or need access to the facilities.
Credentialing is also used in non-medical contexts, including the following:
- Personnel Credentialing: This is when an organization assigns credentials to its employees or vendors.
- Political Credentialing: This term refers to political parties assigning credentials to delegates for party conventions.
Entities That Regulate or Provide Standards for Credentialing of Providers
The federal Centers for Medicare & Medicaid Services (CMS) and the Joint Commision on Accreditation of Healthcare Organizations both require that healthcare providers be credentialed. Healthcare organizations that don’t follow the CMS regulations are not eligible for Medicare or Medicaid reimbursement. Similarly, the Joint Commission accredits only those who follow its regulations. Most U.S. hospitals pursue the Joint Commission accreditation, which is required for Medicare and Medicaid reimbursement eligibility. States also have their own regulations.
Other groups set standards on credentialing as well, and many healthcare organizations follow them to receive additional accreditation. Those groups include the following:
- The National Committee for Quality Assurance (NCQA)
- Utilization Review Accreditation Commission (URAC)
- The Accreditation Association for Ambulatory Healthcare (AAAHC)
- Det Norske Veritas (DNV)
How Does Provider Credentialing Work?
Provider credentialing is the process of establishing that medical providers have proper qualifications to perform their jobs. This requires contacting a range of organizations, including medical schools, licensing boards, and other entities, to verify that the providers have the correct licenses and certificates. In addition, the credentialing organization makes sure there are no past reported issues that suggest the providers are incapable of competently treating patients.
The Primary Phases of Provider Credentialing
The three primary phases of provider credentialing are as follows:
1. Gather Information
- A healthcare facility or health insurance plan asks the provider for information on his or her background, licenses, education, etc. The provider may submit the information in a questionnaire through email or through software.
- In some cases, the healthcare facility or insurance company works with a third-party company — called a credentials verification organization (CVO) — that works with the provider to gather and verify information. Organizations often hire CVOs to allow for more efficient credentialing.
2. Check the Information
- In many cases, the facility or insurance company will do the background work. They will directly correspond with licensing agencies, medical schools, and other entities to verify the provider’s information.
- In other cases, the facility or insurance company may use credentialing software to continuously check information that licensing agencies and other entities make available online. The CVO may also run verification checks.
- Many healthcare organizations use collaboration and work management platforms to help them organize and record provider information and get automatic updates when certain credentials expire or need to be re-checked.
- In all cases, the checks include monitoring reports about medical incidents, malpractice claims, or other information that could raise questions about whether to credential or re-credential the provider.
3. Award the Provider with Credentials
- After the organization verifies all required credentials and finds no negative issues, the healthcare facility awards credentials to the provider.
- After the health insurance company completes a similar process, it can decide to approve the provider as an in-network provider. That is, the insurance company will pay the provider for treating patients who have its insurance.
Common Information Requested to Credential Healthcare Professionals
There is some variance in the information required of healthcare providers by different healthcare facilities and insurance companies. However, the most commonly requested information includes the following:
Name
Previous/other names
Gender
Ethnicity
Mailing address
Email address
Daytime phone number
Citizenship information
Recent photograph
Current CV
Date of birth
Social Security number
Education and training
Residency
Licensing
Specialties
Specialty certificates
Qualifications
Career history
Patient age focus
Languages spoken
Hospital affiliations
Medical group affiliation
Practice address
Practice Tax ID Number
Practice phone number
Primary practice contact
National Provider Identifier (NPI) number
Board certification
Acceptance of new patients
Sanctions or disciplinary actions
Malpractice claims history
Proof of professional liability insurance
Continuing medical education documents
Peer references
Additionally, Davis-Green says healthcare facilities may look more deeply into available statistics that reflect on the provider’s skills, such as mortality rates, rates of patients’ readmissions to hospitals, and similar information. She also considers peer references important. “Sometimes, peers have more insight” into a provider’s skills, along with any possible issues, she says.
The Bottleneck: How Long the Credentialing Process Can Take
All of this verification takes time — even an exceedingly long time.
Under the most efficient circumstances, a physician can be credentialed to work at a hospital or credentialed and approved to be in-network for a health insurance company in 30 days. More often, the process takes 60 to 90 days. And on occasion — especially with insurance companies — it can take six months or more.
Susan Ward is the director of payor enrollment at Symplr. She explains that the process becomes complicated in part because each state has specific credentialing laws and regulations. The process can also take longer for recent medical school graduates as they wait for schools to confirm graduation, or for providers who’ve been sued for medical malpractice, as finding important details on the cases takes time, Ward explains.
In addition, many healthcare groups still use paper or email applications, which they complete and return via fax machines. Only after receiving this paperwork do credentialing employees input the information into computers.
How Lengthy Processes Can Affect Doctors, Hospitals, and Healthcare
A drawn-out process can have a significant financial impact on healthcare providers and hospitals.
When a provider is waiting for hospital credentials, he or she can’t see patients at the hospital. When a provider is waiting for insurance approval of credentials, he or she won’t be reimbursed by the insurance company for seeing patients who have that insurance.
“A physician’s time is money,” says MedSpoke’s Larson. He estimates that “for every day a physician isn’t working, that’s a loss of $7,000 for a hospital. You multiply that over six months, that’s a big chunk of change.”
That’s why it’s important that providers and hospitals ensure the process moves as efficiently as possible, Larson says.
The Council for Affordable Quality Healthcare: A Critical Role in Provider Credentialing
The Council for Affordable Quality Healthcare (CAQH) is a not-for-profit organization formed by some of the nation’s top health insurance companies. One of its online products — formerly called the Universal Provider Datasource and now known as ProView — gathers a common set of information from healthcare providers, including their professional background. Hundreds of insurance plans then use that common information as they credential providers — and relieve providers of the burden of submitting the same information to every insurance company they may want to enroll with.
CAQH’s website says that more than 1.4 million healthcare providers self-report information to ProView.
Completing the CAQH Application: Advice for Physicians or Physician Groups
Experts offer recommendations on completing the CAQH forms, which include the following:
- Don’t complete the CAQH form on paper — complete it online. While CAQH encourages completion of the application online (and most providers do so), it also offers an option to apply on paper and send the materials to CAQH. Experts recommend that you not do that, as CAQH can delay inputting those materials into its online system, which means it takes longer for your information to be available and longer for your credentialing.
- Make sure the provider’s resume is accurate and complete. Take special care to ensure that you format the resume dates as the system asks and that there are no time gaps in the provider’s resume. CAQH will suspend processing of the application until every gap — even a day — is accounted for.
- Have scanned copies of required materials. CAQH will ask you to upload them as part of the application process.
- Make sure the provider “re-attests” every four months. Re-attesting is a simple, quick process of confirming that everything remains accurate in the provider’s profile. When providers don’t re-attest, their profile information is not available to insurance companies, which can delay credentialing with insurance companies.
How to Ensure the Credentialing Process Goes Smoothly
Certainly, credentialing can be a long, tedious process for providers and clinic managers. But experts offer recommendations that can increase the chances of a smooth and moderately quick process. Here are some of those suggestions — whether a provider is completing a CAQH application or answering credentialing questions from a healthcare facility or insurance company.
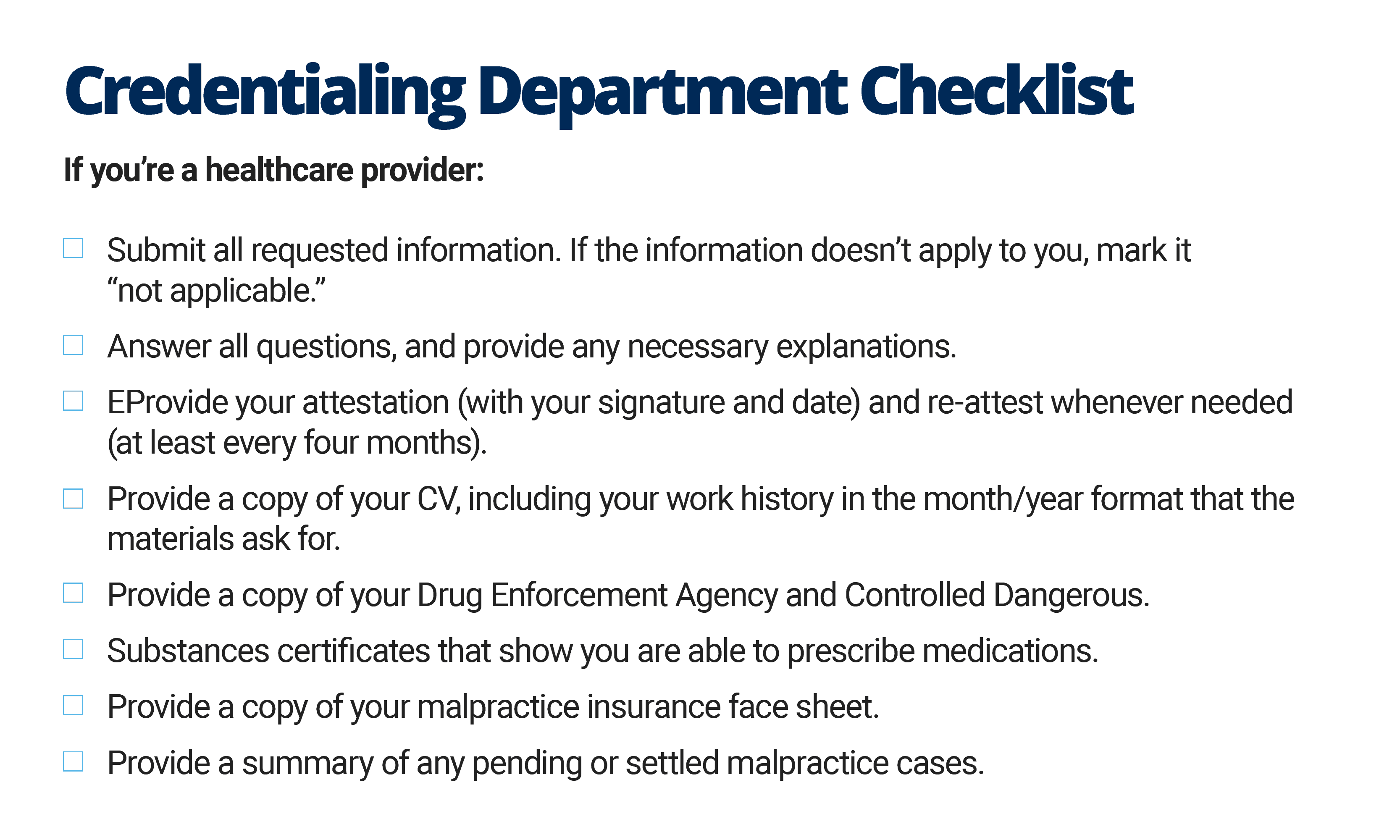
If you’re a healthcare provider:
Download Healthcare Provider Credentialing Application Checklist
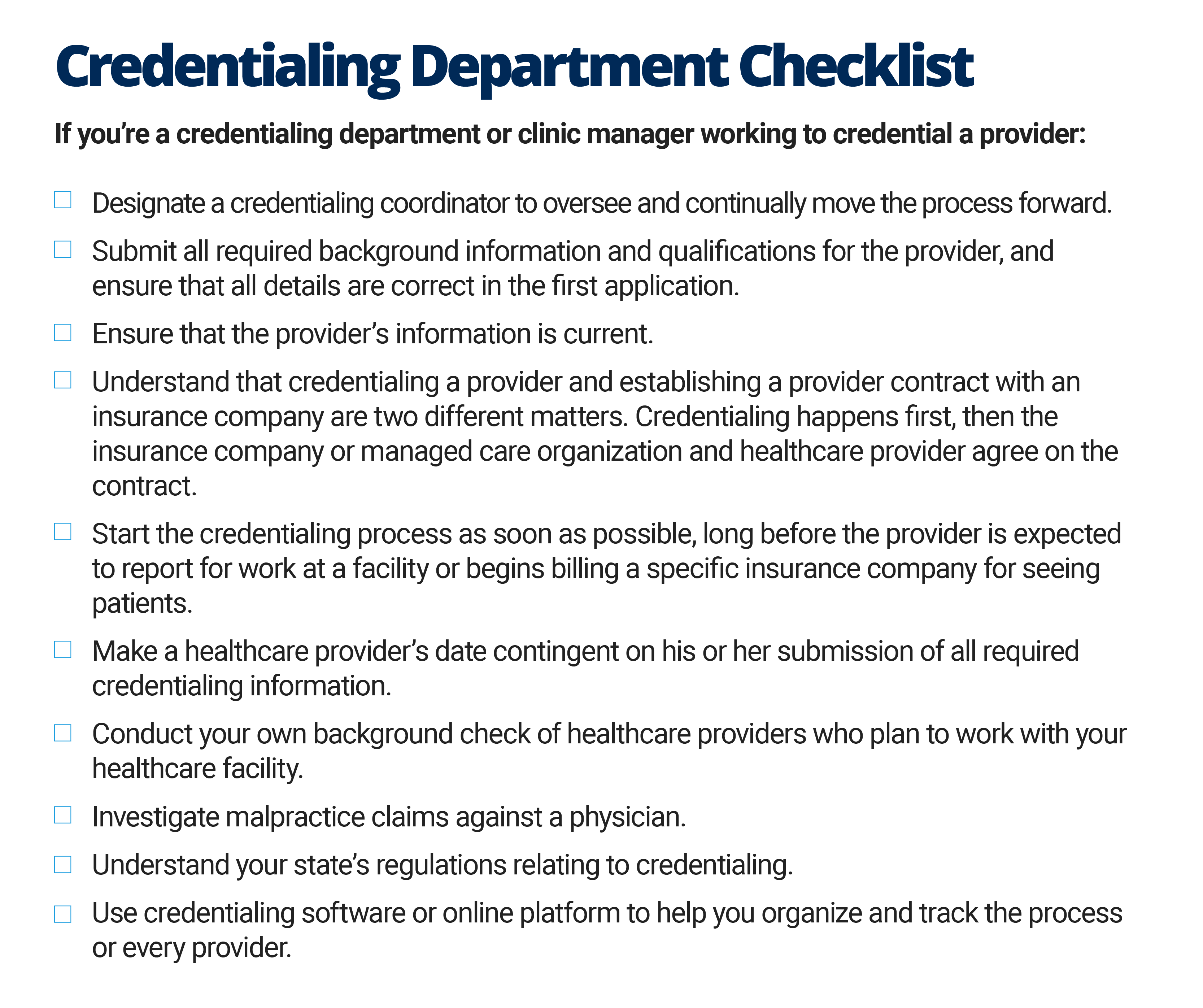
If you’re a credentialing department or clinic manager working to credential a provider:
Download Credentialing Department Checklist
Below are some special considerations for credentialing a provider with insurance companies:
- Ensure the provider completes the CAQH applications accurately.
- Make a list of all insurance companies the provider wants to enroll with, and determine the credentialing requirements for each insurance company.
- Follow up with the insurance company often to check if it needs any information and determine where the application is in its process.
In the end, experts say there are some tricks — and perhaps required persistence — to move along the often halting credentialing process more efficiently.
Davis-Green, the Louisiana healthcare consultant, says that during her work in credentialing organizations, she made sure to become friendly with people at licensing and similar agencies, who can help get information more quickly.
“I was best friends with the executive assistant to the executive director” of the state’s licensing board, Davis-Green says. “It’s all about relationships and finding those people who can get you access to that information in a timely manner.”
Ward, with Symplr, emphasizes the importance of a healthcare facility starting the process early — long before a provider is expected to begin work. On the provider side, she highlights the need for assistants to a healthcare provider to know when they are expected to respond to a request for new information, for instance, and the significance of the process.
Healthcare Credentialing FAQs
How often should healthcare providers be “re-credentialed”?
Healthcare providers need to be re-credentialed at least every three years. Some healthcare facilities or insurance companies perform recredentialing even more often.
Can healthcare providers make corrections in their credentialing information?
Yes, healthcare providers have the right to review all information about them in the credentialing process and can formally offer corrections to erroneous information.
What is primary source verification?
Primary source verification is the requirement that healthcare facilities directly check with the agency granting licenses, certificates, and similar credentials to ensure that the provider has the credential in good standing. For instance, a hospital would directly check with a state licensing board to verify that a physician has a medical license in a particular state.
Does the credentialing process differ depending on the type of provider (doctors, physicians assistants, dentists, nurse practitioners)?
The required credentials and certificates vary among the types of providers, but the process is similar. During the process, the provider submits basic information (Social Security number, date of birth, degrees, and graduation dates). From there, healthcare organizations check with agencies to verify that the provider has the required certificate or license.
What’s the difference between “credentialing” and “privileging”?
Credentialing is the process of checking that healthcare providers have the required licenses, certificates, and other titles in good standing to do their job. A hospital will first check a provider’s credentials to make sure they can work in the facility.
Privileging is when the hospital authorizes the provider to practice certain types of medicine and perform certain procedures at the facility. For example, an obstetrician may have a medical license, but isn’t qualified to perform heart surgery. A hospital grants privileges to a provider, based on his or her medical background and skills.
Often, when hospitals gather information for credentialing, they also gather data that can inform their decision on what privileges to assign the provider.
Discover a Simple, Efficient Credential Tracking Solution in Smartsheet
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team — and adapt as those needs change.
The Smartsheet platform makes it easy to plan, capture, manage, and report on work from anywhere, helping your team be more effective and get more done. Report on key metrics and get real-time visibility into work as it happens with roll-up reports, dashboards, and automated workflows built to keep your team connected and informed.
When teams have clarity into the work getting done, there’s no telling how much more they can accomplish in the same amount of time. Try Smartsheet for free, today.