What Is Patient Management?
Patient management is a broad term, with two categories of definitions. One definition refers to a software tool that streamlines processes within a medical practice or hospital, and the other refers to an entire system of care involving both patient and practice.
Previously, the Food and Drug Administration (FDA) regulated some types of patient management software (PMS): Those used as medical devices (such as a wearable technology) to collect personal data, or those that used data or performed analysis to help a physician diagnose or treat a patient. Instead of handling tasks like booking appointments, checking in patients at an office, or billing, the goal of these systems is to increase patient engagement and help them take an active role in their own health care. In December 2016, however, the FDA changed its regulations and is no longer treating this type of software as a medical device.
Resource and patient management systems (RPMS) combine the medical data and analysis aspects of other software with administrative tools to help make a practice or hospital more efficient. This system combines patient management and health with the medical practice or hospital management. This approach to health care is more than a procedure because it focuses on the relationship between patient and practice and not just an illness.
There are many different names and acronyms for patient management systems like patient information management system (PIMS) or systematic patient management, but they all seem to have the same general goal of streamlining care.
What Do You Manage in Patient Management?
It’s safe to say all patient management tools have something to do with the overall patient experience. Whether it’s an online tool to make appointment booking easier or a way to converse with a physician, practices and hospitals are evaluating their systems.
In medical practices, patients are the customers, and keeping them happy has become a priority. Physicians are also looking for ways to improve patient care and build relationships between office visits. Office staff often need ways to automate administrative tasks and collect information. Patient management can do all that and more, and sometimes save money in the process.
Since Practice Fusion entered the market in 2007, the use of patient management systems has increased from seven to 85 percent, Douglass says. “This industry has moved digitally fairly rapidly. It’s a profound change in how medical and clinical information about patients has evolved over the past ten years.”
Functions and Regulations of a Patient Management System
A patient management system often goes beyond just being an electronic health record or electronic medical record (EMR). Government incentives helped expedite the move towards electronic health records, and many practices realized that other software and systems could be beneficial. Patient management software can integrate appointment history, patient information, diagnoses, prescriptions, billing records, and more. It can also help practices and hospitals reduce costs by automating some tasks like appointment scheduling, sending reminders, and billing.
The 21st Century Cures Act passed Congress in December 2016 and amended the definition of a medical device to exclude certain software functions. Before this law, it was unclear which types of medical software required regulation and often left up to interpretation. Section 3060 of the new law, called “Clarifying Medical Software Regulation,” mentioned five major types of software that no longer require classification. Here are the software types as outlined in Section 3060:
- For administrative support of a health care facility, including the processing and maintenance of financial records, claims or billing information, appointment schedules, business analytics, information about patient populations, admissions, practice and inventory management, analysis of historical claims data to predict future utilization or cost-effectiveness, determination of health benefit eligibility, population health management, and laboratory workflow;
- For maintaining or encouraging a healthy lifestyle and is unrelated to the diagnosis, cure, mitigation, prevention, or treatment of a disease or condition;
- To serve as electronic patient records, including patient-provided information, to the extent that such records are intended to transfer, store, convert formats, or display the equivalent of a paper medical chart, so long as [such records] were created, stored, transferred, or reviewed by health care professionals, or by individuals working under supervision of such professionals [and the software] is not intended to interpret or analyze patient records, including medical image data, for the purpose of the diagnosis, cure, mitigation, prevention, or treatment of a disease or condition;
- For transferring, storing, converting formats, or displaying clinical laboratory test or other device data and results, findings by a healthcare professional with respect to such data and results, general information about such findings, and general background information about such laboratory test or other device, [unless the software] is intended to interpret or analyze clinical laboratory test or other device data, results, and findings;
- Unless the function is intended to acquire, process, or analyze a medical image or a signal from an in vitro diagnostic device or a pattern or signal from a signal acquisition system, for the purpose of:
- Displaying, analyzing, or printing medical information about a patient or other medical information (such as peer-reviewed clinical studies and clinical practice guidelines);
- Supporting or providing recommendations to a health care professional about prevention, diagnosis, or treatment of a disease or condition;
- Enabling such health care professional to independently review the basis for such recommendations that such software presents so that it is not the intent that such health care professional rely primarily on any of such recommendations to make a clinical diagnosis or treatment decision regarding an individual patient.
The new law recognizes that these types of practice management software solutions pose little or no risk to patients, but the FDA does have some authority to regulate new types of software if it deems it necessary.
The clarifications were essential because there were many gray areas under the old laws. Some critics said software reading data from devices could replace the decision and judgment of a physician.
Elements of Patient Management Software
Patient management systems can contain many elements - a major one is computer software. Many different elements make up this kind of software and there are several options and features as well as several brands available that are part of managing the patient experience.
A survey in 2013 from Accenture (a global management consulting, technology services and outsourcing company) states that between 69 and 82 percent of patients said electronic capabilities were at least somewhat important. Of these people, a third to almost a half said online access with their doctors was very important.
The study also found the following statistics from respondents:
- 82 percent wanted access to medical records
- 77 percent wanted to be able to book appointments online
- 76 percent wanted to request prescription refills online
- 74 percent wanted to receive reminders via email or text
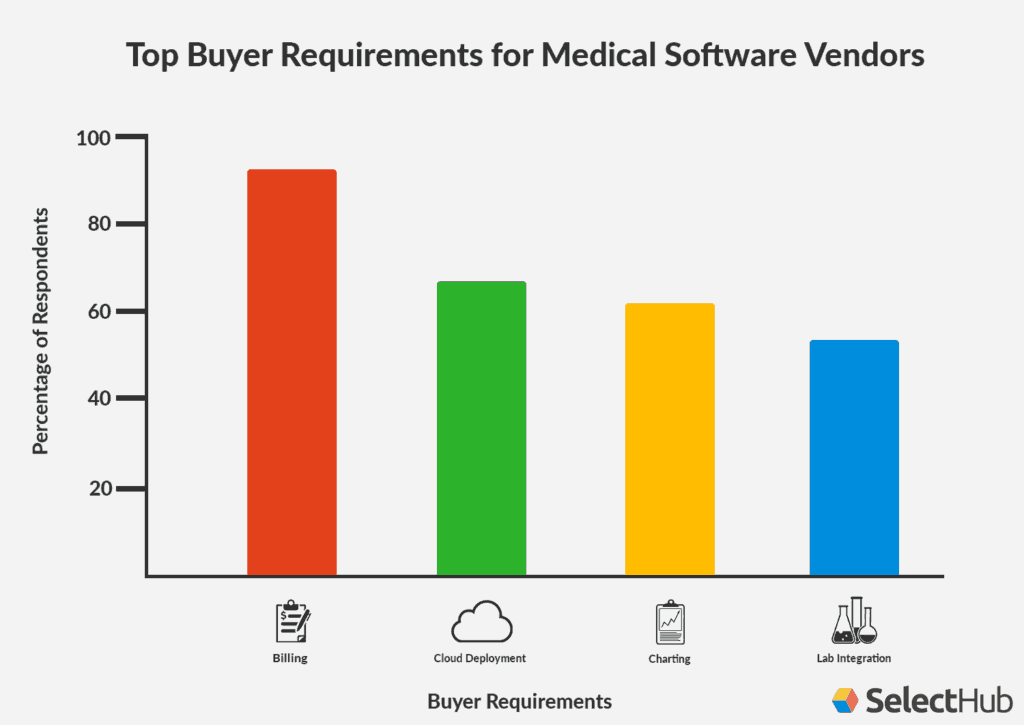
The company SelectHub recently published a study of 100 companies that were shopping for patient management software. “They told us what was most important to them,” explains Michael Shearer, Vice President of Marketing for Denver-headquartered SelectHub.
Shearer says most companies looking for software today are not first-time buyers. “We’re finding more practices are researching replacements. You’re looking more at the second generation of implementing systems,” he adds.
Functionality and needs differ depending whether or not the medical practice is small and independent or part of a larger medical group. PMS systems work entirely differently within a hospital setting. The software can link practices and medical offices so things like patient records are easy to access on a variety of devices in different settings.
- A patient management software system can provide any of the following functions:
- Welcome patients to a practice or hospital and allow people to sign in
- Screen identification and print badges for visitors
- Complete forms before appointments to decrease patient time spent in the waiting room and administrative time spent inputting data
- Keep medical records and allow easy accessibility from a variety of locations including from a mobile device
- Schedule appointments and allow patients to see what is available and pick the best time for them
- Send confirmations of appointments and place them on an electronic calendar
- Send reminders about appointments, hopefully reducing the number of no-shows
- Send follow-up health information, advice, and reminders of what physicians said to do to increase patient participation in their own health care
- Notify physicians when patients arrive to decrease wait times
- Keep records of patient encounters so both physicians and patients can refer to previous conversations and appointments
- Monitor and receive data from medical devices and provide alerts both to physicians and patients if medical attention is necessary
- Allow emails and conversations between patient and physician
- Generate bills and insurance claims
Regardless of the software a medical practice or hospital chooses, it still needs to adhere to HIPAA, the Health Insurance Portability and Accountability Act of 1996. This United States legislation outlines policies and procedures about data privacy and security provisions for medical information. When looking for patient management software, there are a few security and HIPAA compliance factors to consider:
- Is data transmitted with encryption?
- Are servers housed in secure locations with backup plans and disaster recovery systems?
- How are users verified?
- How is data stored?
- Are the firewalls strong?
All of the elements are things to consider when looking into patient management tools. Remember, patient management is much more than a piece of software: It’s about taking everything into account from the moment a patient walks in the door to interactions after that patient leaves.
Potential Benefits of Patient Management for Medical Practices and Hospitals
Paying attention to patient management can have many benefits for medical practices and hospitals. Speeding up communications and administrative tasks reduces administrative staffing time and allows staff to focus on direct patient care. The amount of time spent on data entry, record keeping, and appointment reminder phone calls is also reduced.
“Nobody wants to wait, it’s a wasted resource,” USC’s Belson says, adding there is a lot of room for improvement in healthcare. Forms are one example: When you visit a doctor’s office, you sign in and fill out a form. You then answer some of those same questions for a nurse, and then maybe again for the doctor. A streamlined admittance process can eliminate some of these redundancies.
Download Patient Sign-in Sheet Template
Smaller practices with limited resources can especially benefit from such a system because it minimizes administrative staff time and can potentially link practices together to create larger health systems. Data analysis can help practices or hospitals change policies and procedures if something is not working as effectively or efficiently as it should.
“They’re kind of all the same, a doctor’s office is a doctor’s office, a hospital is a hospital,” Belson explains. Collecting and analyzing similar data from various locations can help identify possible gaps and inefficiencies. “If you measure that and compare it to other places, it tells you where you need to focus your attention,” he says.
Software can link electronic health records with practice management tools to help with things like immediate record transfers between medical practices, hospitals, and other care centers, as well as automate electronic prescribing and data analysis. Connecting to patient management systems from a mobile device is also useful when determining physician on-call schedules and accessibility.
Going electronic creates a cleaner and less-cluttered office, and also reduces treatment errors that result from incomplete paper records. Another bonus of going digital is that it eliminates the potential of misinterpreting bad handwriting.
Capitalizing on the incentives that come from recent billing changes to Medicare and Medicaid as part of the Affordable Care Act and adopted by many insurance companies can help keep a patient healthy and prevent illness. Douglass uses an example of a pre-diabetic patient. With paper charts, there is no efficient way to tell which patients had not had specific blood sugar tests or seen a doctor recently without looking through every chart. “Some practices tried, but found it was not cost effective to do that,” Douglass says. With the data from a practice management system, office staff can quickly identify which patients need a visit to the practice. “Fast forward to today and a practice can ask that question and get an answer in literally 10 seconds,” Douglass explains.
Backup systems are also easier when everything is electronic. Many software system providers offer cloud backups that make it easier to restore systems in the case of a hardware failure. Some systems, like Practice Fusion, are entirely cloud-based. In the event of a natural disaster like a flood or a storm, physical records might be damaged or destroyed, but electronic ones will remain intact. There is also a high level of security and privacy protection necessary to comply with HIPAA regulations.
Scheduling appointments electronically can have many benefits for practices because patients can see available appointment times and select the times they want instead of going back and forth with someone on the phone. The software can also send voice, email, and text reminders about appointments, which can greatly reduce the number of no-shows.
Patient Management System Benefits for Physicians
A physician’s main goal is the overall health and wellness of a patient. Achieving that takes teamwork, and efficient and effective patient management can help. Although implementing new systems costs money and often has a learning curve, the results can be an asset to patients, not just an expense.
Because some administrative tasks handled by staff can be handled by technology, staff morale in medical offices can improve because of a decreased manual workload. Most patient management systems integrate with electronic medical records and electronic health records so a physician has quick access to someone’s entire medical history. Physicians can also communicate directly with patients to clarify care instructions or diagnosis, or to monitor their progress towards health goals. Healthcare providers can respond when it is convenient for them and can provide educational materials if necessary. Systems can also automatically remind patients about advice from their physicians. Linking to labs can also expedite issuing test results for patients.
Specialists can also communicate with other doctors to coordinate care and recommendations for patients. If some medical devices are part of a patient’s care plan, medical offices can monitor that data and intervene when needed. This data and monitoring can help drive treatment decisions, especially in patients with chronic conditions.
“Very often, we see skepticism from doctors and that skepticism is completely abated after three to six weeks because they see how a web-based system can be more efficient for their practice,” Douglass says. His company’s system links medical practices with labs, pharmacies, specialists, and more. Practice staff does not need to keep calling labs for test results or corresponding with pharmacies about prescription questions. Practice management systems can do that automatically and the correspondence goes both ways, both in and out of the practice. “The administrative time in a practice is as important as a physician’s time,” Douglass says.
Benefits of a Patient Management System for Patients
From the perspective of a patient, patient management software treats them more like consumers and less like sick people. Software can fill gaps and empower patients to work with their own time schedule and not that of the physician’s office.
Many patient management systems allow patients to do the following:
- Schedule appointments
- Refill prescriptions
- Ask questions
- Get appointment and treatment reminders electronically, using email or text
Douglass believes management systems can keep staff from constantly shuffling papers around while talking to a patient, which makes the patient compete for attention. “It’s more of a personal experience for patients because when they’re interacting with the front office staff, they’re interacting one-on-one,” Douglass says. “It seems more professional to the patient.”
Allowing patients to handle some tasks on their own and often after regular business hours can improve their overall morale and increase satisfaction with a physician’s office or practice. Patients can also check their own records and look at test results. They can scan for possible mistakes and ask for a correction, both of which are parts of a patient actively participating in their own health care. In some cases, patients can choose to connect data from wearables to their physicians, which can increase the feeling of a team working on behalf of the patient.
Potential Drawbacks of Patient Management
Since, as of January 1, 2014, all medical practices accepting insurance are required to use electronic medical records to maintain existing Medicaid and Medicare reimbursement levels, many practices are choosing to deploy full practice and patient management software.
While the benefits may outweigh the drawbacks, it’s important to be aware of potential challenges. As with any software, hacking is a possibility so security is critical. Transmission of computerized physician order entry (CPOE) can also be a security concern. CPOE is a form of patient management software since it deals with the care and processes of patients. With this process, a medical practitioner enters instructions about medical care or treatment and transmits that information over a computer network to other departments. This practice is common in hospitals, so their network security is essential.
Another past criticism of patient management involved the number of regulations in place. However, since the passage of the the 21st Century Cures Act in 2016, many of those regulations regarding patient management software as a medical device do not exist anymore. Critics used to say those regulations stifled innovation because vendors would not want to create new products if they knew they could be stuck in regulatory bureaucracy.
Cost can also be a drawback for patient management systems, and choosing the wrong one can be a costly mistake. “I highly advocate for doing a trial if it is available, try it before you buy it,” SelectHub’s Shearer advises.
Improve Patient Management with Smartsheet
Empower your people to go above and beyond with a flexible platform designed to match the needs of your team — and adapt as those needs change.
The Smartsheet platform makes it easy to plan, capture, manage, and report on work from anywhere, helping your team be more effective and get more done. Report on key metrics and get real-time visibility into work as it happens with roll-up reports, dashboards, and automated workflows built to keep your team connected and informed.
When teams have clarity into the work getting done, there’s no telling how much more they can accomplish in the same amount of time. Try Smartsheet for free, today.